EULAR Annual Scientific Meeting 2023
Alexandra Ladouceur, Lourdes Gonzalez Arreola, Shahin Jamal, Marie Hudson, Janet
Pope, Sabrina Hoa, Janet Roberts, David Moon, Ammana Karmali, Tatiana Nevskaya, Emma Schmidt1, Nader Toban, Lindsay Cho, Thomas Barnetche, Carrie Ye
Title:
Outcomes and Predictors of Chronic Immune Checkpoint Inhibitor Induced Inflammatory Arthritis: Data from the Canadian Research Group of Rheumatology in Immuno-Oncology (CanRIO) Retrospective Cohort
Background:
Immune checkpoint inhibitors (ICI) improve overall survival and progression-free survival in many types of malignancies and are the new pillar of cancer treatment1. ICIs harness a patient’s own immune system to fight their cancer. However, this activation of the immune system can result in off-target immune-related adverse events (irAEs). One of the most disabling irAE is inflammatory arthritis (ir-IA)2 affecting up to 7.5% of those treated with ICI3. Unlike most irAE which usually resolve within a few months, ir-IA can become chronic and persist even after ICI cessation, requiring long term immunosuppression4. The factors associated with chronic ir-IA and its significance regarding tumor outcomes remain largely unknown. With the increasing use of ICI in the adjuvant therapy, it is important to understand predictors and outcomes of chronic ir-IA in order to best counsel patients.
Objectives:
To determine predictors and outcomes of chronic ir-IA in cancer patients exposed to ICI.
Methods:
The CanRIO group, established since 2018, includes 9 academic sites in Canada and aims to describe the clinical presentation, management and outcomes of patients who developed rheumatic irAE (Rh- irAE) or those with pre-existing autoimmune diseases exposed to ICI using standardized data collection. The sites pooled data to develop a retrospective cohort of patients identified as having a Rh-irAE. We identified patients who developed ir-IA defined by new onset joint tenderness or synovitis in the absence of pre-existing rheumatic disease and who had at least 3 months of follow- up following ICI cessation. Chronic ir-IA was defined as having either persistent symptoms of ir-IA or the continued use of prednisone or DMARDs 3 months after ICI cessation.
Results:
The CanRIO Retrospective Cohort included 193 ir-IA individuals of which 54 met our inclusion criteria. Forty-five of 54 (83%) had chronic ir-IA. Fifteen (33%) were female. Nineteen (42%) patients with
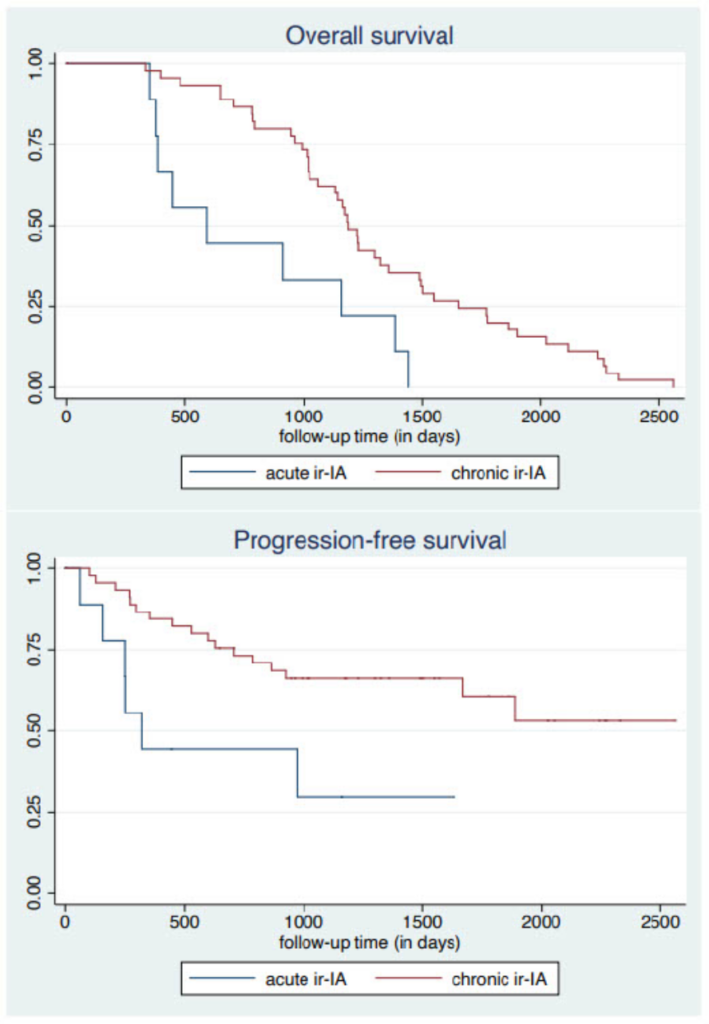
chronic ir-IA had melanoma, 14 (31%) lung cancer and 8 (18%) genito-urinary cancer. Thirty-three (73%) were treated with anti PD-1/PD-L1, 14 (31%) with combination and none with anti-CTLA-4 only. Thirty-five (78%) were treated with conventional DMARDs and 1 (2%) with biologic DMARDs. Univariable logistic regression showed that ir-IA was more likely to become chronic in those with peripheral synovitis compared with those who did not have peripheral synovitis at presentation, (Table 1). Patients with chronic ir-IA had greater overall survival and progression-free survival compared to those with acute ir-IA (log rank tests, p<0.01), (Figure 1).
Conclusion:
A large proportion of ir-IA becomes chronic. The presence of synovitis at presentation is associated with arthritis persistence. Ir-IA is associated with improved overall survival and progression-free survival.
References:
1. Sharma, P., et al., Cancer Discov, 2021.
2. Roberts, J., et al., Autoimmun Rev, 2020.
3. Suarez-Almazor, M.E., et al., Support Care Cancer, 2020.
4. Braaten, T.J., et al., Ann Rheum Dis, 2020.
Table 1. Logistic regression model: univariable analysis to assess factors associated with chronic ir-IA compared with acute ir-IA
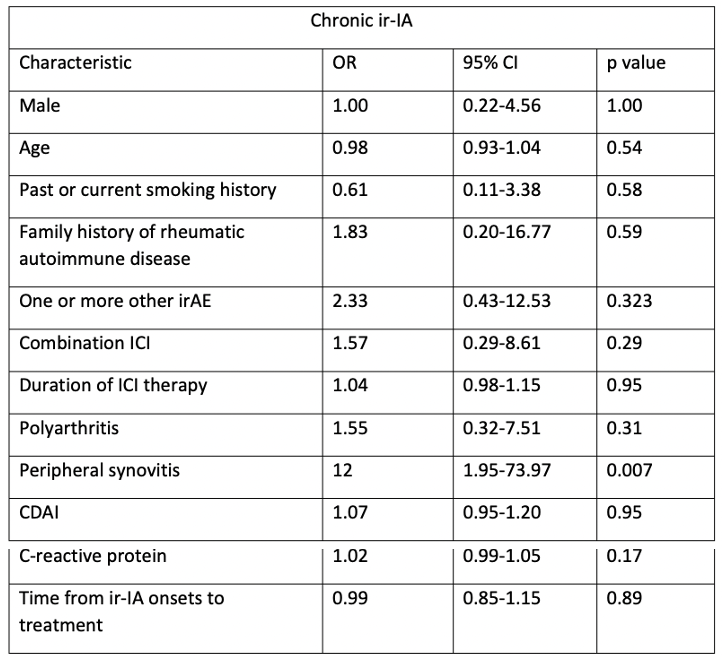
Legend: irAE: immune-related adverse event; ICI: immune checkpoint inhibitors; CDAI: clinical disease activity index
Figure 1. Kaplan-Meier curves for overall survival and progression-free survival based on acute and chronic ir-IA